 |
| A Frozen Addict from 1982. Source: Neurology Update. |
In the 1970s chemists in the illicit drug business began exploring a new class of psychoactive drugs, which were structurally related to the synthetic opiate Demerol. The following story is truly one-in-a-million. It encompasses the first "designer drug" (1) and the organic chemistry used to make it, what can (and did) happen when a reaction procedure is not followed properly, and a deeper understanding of the molecular mechanism of Parkinson's Disease.
The story began in 1947, when Demerol was discovered at Hoffman-La-Roche. At that time, drug companies were searching for pain-killing drugs that did not have the baggage of standard opioid drugs, such as hydrocodone, and oxycodone (2). In fact, MPPP, which is considered to be the first designer drug, was also discovered at Roche around that time, but, unlike Demerol, it was never approved.
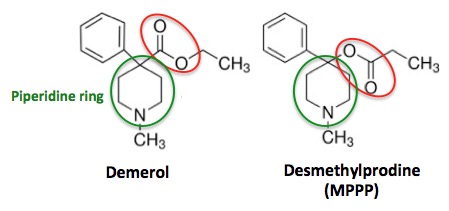 |
| The chemical structures of Demerol (L) and Desmethylprodine (R) |
Even people with little or no chemistry knowledge can see that these two molecules are nearly identical in structure. The only difference is a functional group (red circle) that is found on the piperidine ring (green circle). In Demerol, the carbonyl group (carbon double bond to oxygen) is attached to the piperidine ring. But in MPPP, an isomer (2) of Demerol, the carbonyl group and oxygen atom are switched, so that oxygen is attached to the piperidine. While this may seem like a trivial difference, chemically it is anything but—something that Barry Kidston, a chemistry grad student, would find out the hard way in 1976.
Kidston was interested in finding legal narcotics for his own use. Since MPPP, which has morphine-like properties, was neither approved, nor designated as a Schedule I drug (3), it was perfectly legal to make or use—something that Kidston did for months. Then he got a little sloppy with his chemistry, and the results were disastrous. The disaster was simply a matter of the failure to control the temperature of the reaction that made MPPP. For organic chemists, what followed was not only logical, but predictable. What happened after that was anything but.
 |
| Barry Kidston Photo: Bluelight.org |
The chemical reaction below shows the final step in the MPPP synthesis (from its precursor HPMP- easy to make). It is a common, trivial procedure called acylation.
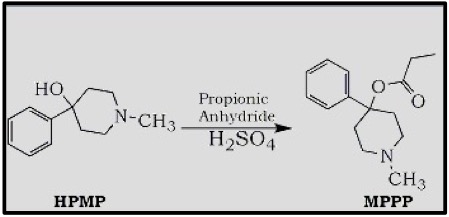 |
| Synthesis of MPPP- Reaction temperature is kept below 30o C (Source erowid.org) |
Any organic chemist will tell you that the the bond shown in green (below) is just dying to break, and it doesn't take much to give it its wish. A little extra heat and that bond breaks, and through a process called elimination, the propyloxy group (orange circle) departs and is replaced by a carbon-carbon double bond (blue circle). Then, instead of MPPP, you have MPTP.
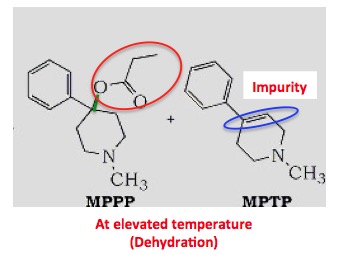 |
| MPTP impurity formed at higher temperatures |
If you're asking yourself "what's the harm in having a bit of an impurity in there?" the answer is "usually not much." But in this particular case, the impurity did something strange and unexpected with help from the brain, which is why this story is so unique.
Any experienced medicinal chemist will look at the structure of MPTP and know that it is very likely to have the properties that will allow it to cross the blood-brain barrier, which it does. This is when the troubles begin. MPTP itself isn't particularly toxic, but it gets metabolized in the brain to MPP+, which is something that you do not want in your brain. Unfortunately for Kidston, he was the lab rat who would inadvertently provide the science world with a fascinating, but deadly lesson in neurochemistry. Shown below is the metabolism that is responsible for a previously-unheard of event:
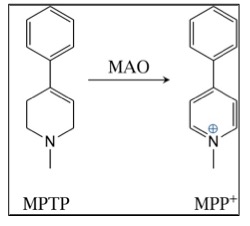 |
| Oxidation of MPTP to MPP+ by momamine oxidase in the brain |
A ubiquitous enzyme called monoamine oxidase (MAO) is responsible for the formulation and metabolism of multiple neurochemicals. It plays a crucial role in regulation of the central nervous system. In this case, the MAO in the brain "saw" MPTP and didn't "like" it, so it oxidized it to MPP+. Assuming that enzymes can make "mistakes," this is one a doozie because MPP+ is seriously bad news. It is now known that it has a particular fondness for the cells in the region of the brain called the substantia nigra. And once it gets there, all hell breaks loose (4). MPP+ specifically kills the dopaminergic neurons in the substantia nigra, where dopamine is normally made. The absence of dopamine is the hallmark of Parkinson's.
The bad batch of MPPP that Kidston injected into himself resulted in the development of strange symptoms within a few days. He experienced bradykinesia—a severe slowing of movement. It became so bad that Kidston was admitted to a hospital where he was diagnosed with Parkinson's Disease, which is very rare in young people. Nonetheless, Kidston did get Parkinson's—from a single injection of an impure drug.
Doctors tried a variety of neuroleptic drugs with no success, and then used L-dopa, which was first tried on Parkinson's patients (with mixed success) in the 1960s. It worked on Kidston, at least for a while. L-dopa loses effectiveness with time. This happened to Kidston, who became severely depressed and died of a cocaine overdose 18 months later.
The link between MPTP and Kidston's Parkinson's Disease was determined by analysis of the residue of drug that remained on the glassware he used. The impurities were isolated, identified and tested. Kidston has unknowingly written a chapter on the neurochemistry of Parkinson's Disease at his own expense.
The MPP+ story did not end with Kidston. In California in 1982, a cluster of six drug users who had taken "China White" (5) all came down with Parkinson-like symptoms (6). When the drug was analyzed, there it was—MPTP, which was a result of a drug dealer trying to do organic synthesis in his garage. The reason for the term "frozen addicts" could not be more clear:
Organic synthesis is both science and art—something that anyone who takes street drugs should consider. It requires both skill and experience to get it right. A drug dealer working in a garage is probably not going to get it right.
Organic synthesis is both science and art—something that anyone who takes street drugs should consider. It requires both skill and experience to get it right. A drug dealer working in a garage is probably not going to get it right.
Notes:
(1) Although there is no strict definition of a designer drug, it usually refers to a new drug that is derived by synthetic modification of a psychoactive legal, approved drug.
(2) Neither has anyone else. There are still no good alternatives to opioids for moderate-to-severe pain.
(3) Isomers are chemicals that have the same molecular formula, but different structures and (usually) different properties.
(4) Schedule I drugs are not approved for use in people and have a high addiction potential.
(5) China White is one of the street names for fentanyl, the drug that is now killing opioid addicts in droves.
(6) Almost anyone looking at the chemical structures of MPP+ and the herbicide paraquat (below) would conclude that they would act in a similar manner. That is how similar their structures are. But they do not. Paraquat's primary toxicity is in the lungs. This is almost certainly due to the fact that the herbicide does not have properties that would allow it to cross the blood brain barrier (not even close). Neither does MPP+, but keep in mind that MPP+ enters the brain as its precursor MPTP, which has just the right properties to do so.
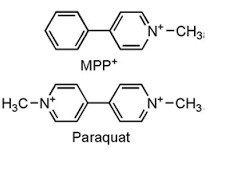 |
The chemical structures of MPP+ and Paraquat—an eerie resemblance.
Source: Science and Education Publishing
|
No comments:
Post a Comment